Blog Post
Insight: The Clash of the Pandemics: The Need for Chronic Disease Prevention
By: Andrea Thomas Brandley
Note: The opinions expressed are those of the author alone and do not reflect an institutional position of the Gardner Institute. We hope the opinions shared contribute to the marketplace of ideas and help people as they formulate their own INFORMED DECISIONS™.
Oct 11, 2021 – COVID-19, coronavirus, vaccines, Delta variant, and masks are now common (and tired) words in many conversations. The pandemic has become engrained in our daily lives. But before we’d heard any of these words, public health professionals and researchers were sounding the alarm of another pandemic: chronic disease. And regrettably, the two pandemics have become entwined. Many chronic diseases, such as chronic kidney disease, chronic lung disease, heart conditions, and diabetes, are associated with individuals having a higher risk of experiencing severe outcomes from COVID-19.[i]
For example, diabetes is the second most common underlying condition in COVID-19 deaths nationwide.[ii] And as noted above, individuals with type 2 diabetes and other chronic conditions face a greater chance of experiencing severe complications if they contract COVID-19. Results from one study found 1 in 5 hospitalized COVID-19 patients with diabetes needed a ventilator within seven days of admission, and updated results found 1 in 5 died within 28 days of admission.[iii], [iv] Another study showed hospitalizations were six times higher and deaths 12 times higher among COVID-19 patients with underlying conditions compared with those with none.[v]
In Utah, 71.6% of hospitalized cases had an underlying condition (where pre-existing conditions were known). Diabetes is the second most common of these conditions, manifesting in 26.8% of hospitalized cases.[vi]
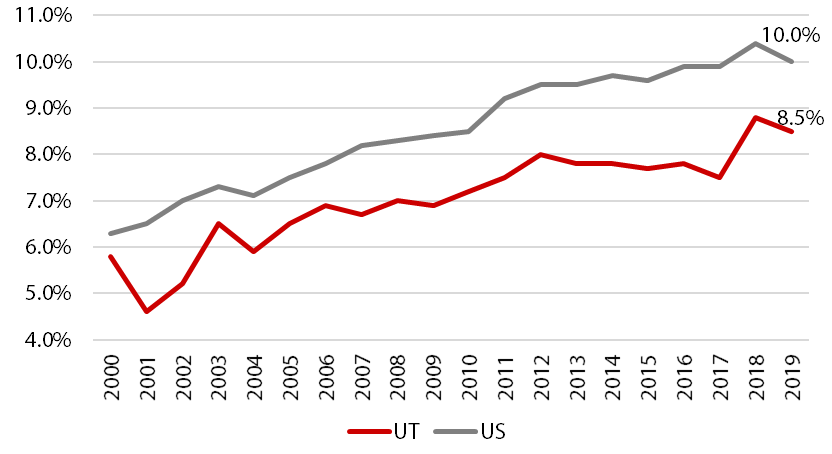
Unfortunately, rates of diabetes have risen dramatically over the last several decades. Less than 1% of the U.S. population had diagnosed diabetes in 1960 compared with 6.8% of the population in 2018.[vii], [viii] Figure 1 shows diabetes prevalence for adults from 2000 to 2019 in Utah and the U.S., with 2019 rates of 8.5% and 10.0% respectively. While Utah’s prevalence is lower than the U.S., it rose nearly three percentage points from 2000 to 2019. As Utah’s demographics continue to change, and our population ages, chronic disease prevalence may increase.
Figure 1: Adult Diabetes Prevalence in Utah and the U.S., 2000‒2019
Note: Age-adjusted. Utah BRFSS updated their methodology for age adjustment for increased precision. Data have been updated from 2011 onward in all chart views to reflect this change. The “old” methodology is shown from 2000–2010.
Source: Behavioral Risk Factor Surveillance System, Office of Public Health Assessment, Utah Department of Health, Division of Behavioral Surveillance, CDC Office of Surveillance, Epidemiology and Laboratory Services. Retrieved Monday, 4 October 2021 from the Utah Department of Health, Indicator-Based Information System for Public Health Web site: http://ibis.health.utah.gov.
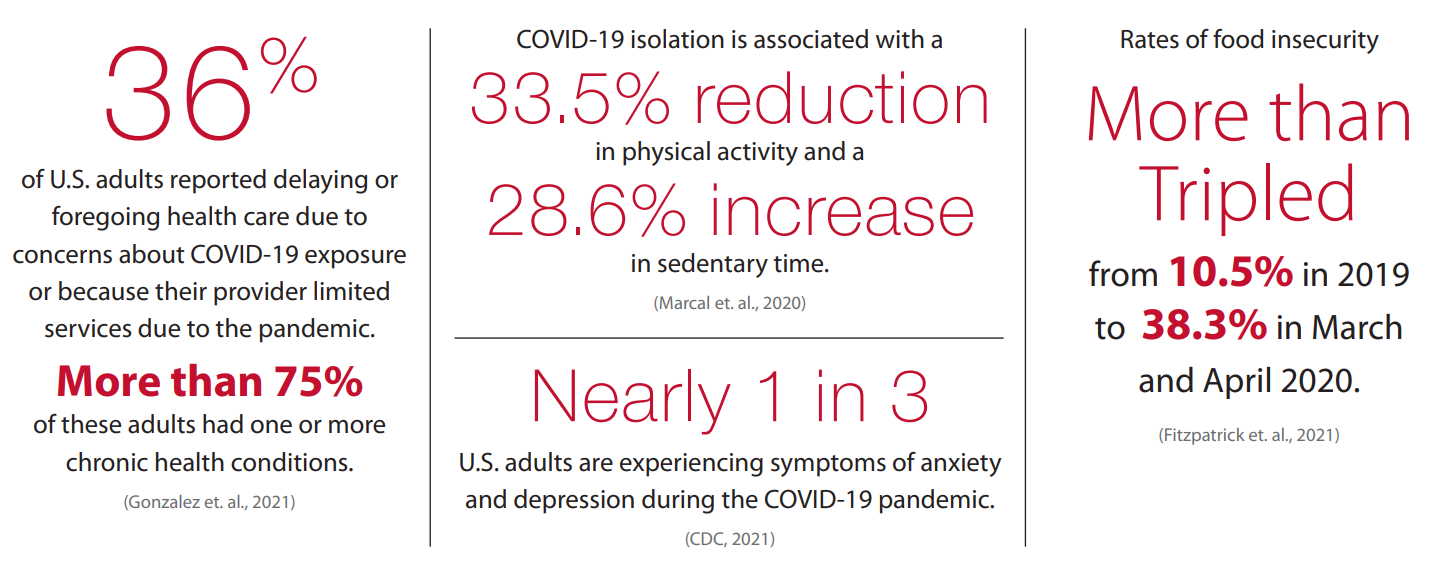
In addition to the direct risk of severe illness associated with COVID-19, people living with diabetes are also at higher risk for experiencing negative impacts from quarantines, school closures, and other disruptions. Many indirect impacts from the public health emergency could worsen the condition of individuals living with diabetes, type 2 diabetes and prediabetes. Some of these impacts are summarized in Figure 2.
Figure 2: Indirect Impacts of COVID-19
The clash of the COVID-19 and chronic disease pandemics underscores the need for continued chronic disease prevention and management. Many prevention programs can help reduce both the onset of type 2 diabetes and other chronic diseases as well as help address some of the indirect risk factors intensified by the public health emergency. Prevention of chronic disease could ameliorate the impacts of COVID-19 and potential future pandemics, improving the health and well-being of Utahns and others worldwide.
Learn more about the connection between COVID-19 and type 2 diabetes here.
Andrea Thomas Brandley is a research associate at the Kem C. Gardner Policy Institute.
[i] Centers for Disease Control and Prevention. (2021). COVID-19: Medical Conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
[ii] Stokes, E., Zambrano L., Anderson, K., Marder, E., Raz, M., Felix, S., Tie, Y., & Fullerton, K. (2020). Coronavirus Disease 2019 Case Surveillance—United States, January 22–May 30, 2020. MMWR Morbidity and Mortality Weekly Report. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7302472/
[iii] Cariou, B., Hadjadj, S., Wargny, M., Pichelin, M., Al-Salameh, A., Allix, I., Amadou, C., Arnault, G., Baudoux, F., Bauduceau, B., Borot, S., Bourgeon-Ghittori, M., Bourron, O., Boutoille, D., Cazenave-Roblot, F., Chaumeil, C., Cosson, E., Coudol, S., Darmon, P., Gourdy, P. (2020). Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. Retrieved from https://doi.org/10.1007/s00125-020-05180-x
[iv] Wargny, M., Potier, L., Gourdy, P., Pichelin, M., Amadou, C., Benhamou, P, Bonnet, J., Bordier, L., Bourron, O., Chaumeil, C., Chevalier, N., Darmon, P., Delenne, B., Demarsy, D., Dumas, M., Dupuy, O., Flaus-Furmaniuk, A., Gautier, J., Guedj, A., Jeandidier, N. (2021). Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study. Diabetologia. Retrieved from https://doi.org/10.1007/s00125-020-05351-w
[v] Stokes, E., Zambrano L., Anderson, K., Marder, E., Raz, M., Felix, S., Tie, Y., & Fullerton, K. (2020). Coronavirus Disease 2019 Case Surveillance—United States, January 22–May 30, 2020. MMWR Morbidity and Mortality Weekly Report. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7302472/
[vi] As of October 2, 2021. Utah Department of Health. COVID-19 Data. Risk Factors. https://coronavirus.utah.gov/case-counts/
[vii] Centers for Disease Control and Prevention Division of Diabetes Translation. (2017). Long-term trends in Diabetes. https://www.cdc.gov/diabetes/statistics/slides/long_term_trends.pdf
[viii] Centers for Disease Control and Prevention Division of Diabetes Translation. Diabetes Atlas. https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html