Blog Post
Insight: The Intersection of Housing and Health Care
By: Laura Summers
Note: The opinions expressed are those of the author alone and do not reflect an institutional position of the Gardner Institute. We hope the opinions shared contribute to the marketplace of ideas and help people as they formulate their own INFORMED DECISIONS™.
Oct 31, 2022 – The Kem C. Gardner Policy Institute recently hosted a Newsmaker Breakfast where several of Utah’s health care leaders discussed the critical health issues facing Utahns today, what’s being done to address them, and how best to prepare for our state’s future health care needs—particularly as our population continues to change and grow.
It was a great conversation and one of the things that struck me after was that “non-traditional” health issues, such as behavioral health, a person’s wellbeing, and the importance of addressing the social determinants of health (a person’s social and physical environment, behaviors, and economic stability) were mentioned almost as frequently as, if not more than, “traditional” health care issues.
These issues weren’t treated separately from the discussion, or as a side note, but were embedded as naturally in a health care discussion as you might imagine diabetes care or cancer treatment would be. The concept of addressing a person’s social determinants of health to improve their health outcomes started to be talked about more widely in the early 2000s and our recent Newsmaker Breakfast indicated to me that the concept is becoming more mainstream and understood, not only by the health care industry, but also by the broader community.
Figure 1: Social Determinants of Health
This aligns with preliminary findings from a series of discussion groups the Gardner Institute has been hosting as part of an assessment of Utah’s behavioral health care system. Housing is one of the most frequently mentioned system gaps and challenges in these discussions. While not surprising, especially given the state of Utah’s current housing market, it is interesting that one of the most frequently cited challenges in Utah’s behavioral health system is something completely external to the system itself.
The lack of housing that is affordable in our state not only creates stress and instability that negatively impact a person’s health, behavioral health, and wellbeing, but it limits the ability to provide necessary behavioral health services such as supportive housing. It is also exacerbating our state’s existing behavioral health workforce shortages. Behavioral health systems across both urban and rural areas in Utah have noted that they are having a difficult time attracting talent to their areas due to the lack of available housing that is affordable.
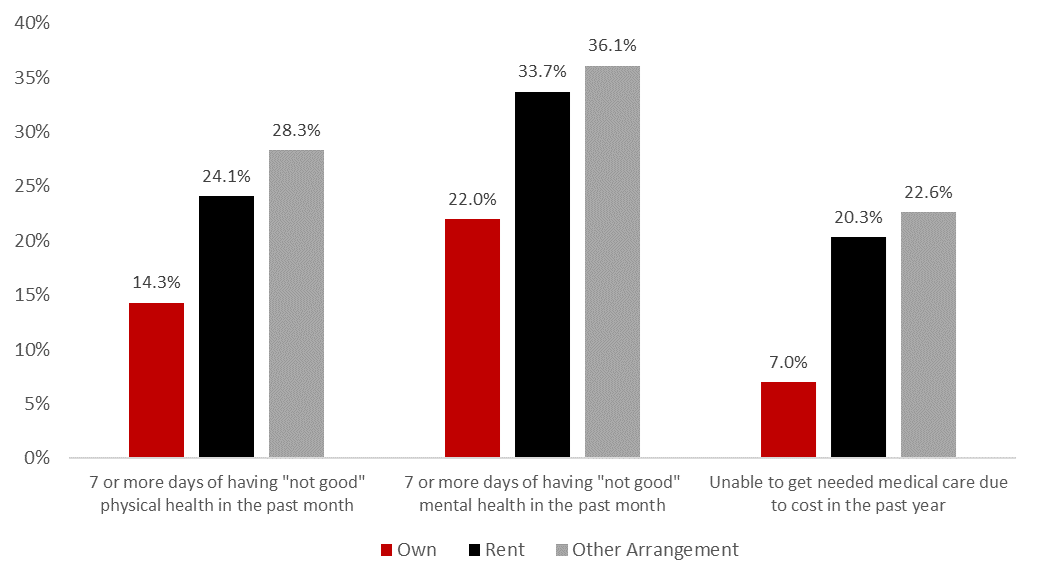
To me, these discussion groups illustrate the important role housing plays in health care. We know that housing is a key factor in improving the financial well-being and economic security of families, and research is increasingly showing that housing stability, safety, and affordability impact health outcomes as well. Figure 2 shows select health indicators by home ownership status for adults in Utah. Homeowners generally experience better physical health, mental health, and better access to health care. In particular, the third set of columns in Figure 2 show that renters and adults living in other arrangements (e.g., group homes, staying with friends or family without paying rent, etc.), are nearly three times as likely to be unable to get needed medical care due to cost than homeowners.
Figure 2: Utah Adult Health Care Indicators by Home Ownership Status, 2021
Note: Other arrangement may include group home, staying with friends or family without paying rent.
Source: Utah Behavioral Risk Factor Surveillance System, Office of Public Health Assessment, Utah Department of Health. Retrieved Mon, 17 October 2022 from the Utah Department of Health, Indicator-Based Information System for Public Health Web site: http://ibis.health.utah.gov.
Clearly there are other factors influencing the numbers above, many of which are outlined in Figure 1. Home ownership is closely tied to economic stability, which is closely tied to educational outcomes, which is influenced by where you live and what schools you attend. This highlights the interconnectedness of a person’s social determinants of health and how important they are in influencing their health outcomes.
Research is also emerging that shows how important addressing housing stability is in terms of directly improving a person’s health. In 2009, the Camden Coalition implemented its Camden Core Model, which connected patients with complex health needs to a care team comprised of nurses, social workers, and community health workers who provided direct medical care, care support, and assistance with accessing social supports in an effort to improve patients’ health. Unfortunately, an evaluation of the program did not find any meaningful differences in hospital readmission rates between patients who received the intervention and those who did not.
As the Camden Coalition has sought to better understand why, one of the issues that emerged was the fact that many of the patients in the intervention group lacked stable housing, and therefore could not receive home visits (which have a direct impact on reducing hospital readmission rates for those recently discharged from the hospital). Until these patients could be connected to stable, affordable housing, their health generally did not improve (as measured by readmission rates).
Housing affordability is not an easy issue to address, particularly during periods of rising interest rates, rapid population growth, increasing demand for housing, and increasing prices, all of which Utah has experienced in recent years. The persisting issues of housing affordability facing our state, though, may continue to create negative reverberations throughout the state’s health and behavioral health systems that can’t be addressed by health care systems’ reforms alone.
Laura Summers is the senior health care analyst at the Kem C. Gardner Policy Institute.