Blog Post
Insight: COVID-19 Spotlights Racial and Ethnic Health Disparities in Utah
By: Andrea Thomas Brandley
Note: The opinions expressed are those of the author alone and do not reflect an institutional position of the Gardner Institute. We hope the opinions shared contribute to the marketplace of ideas and help people as they formulate their own INFORMED DECISIONS™.
Oct 25, 2020 – As COVID-19 continues to spread, data reveal unequal impacts across population groups. Communities of color nationwide have been hit hard by the coronavirus, and Utah is no exception. The Hispanic/Latino population is Utah’s largest minority group. While they make up 14.2% of the state’s population, they account for 29.5% of COVID-19 cases and 20.9% of COVID-19 deaths.[i] Inequities in social determinants of health likely contribute significantly to this overrepresentation.
The Centers for Disease Control and Prevention (CDC) defines social determinants of health as “conditions in the places where people live, learn, work, and play that affect a wide range of health and quality of life risks and outcomes”.[ii] These conditions contribute to adverse health effects for communities of color. Some of these factors include:
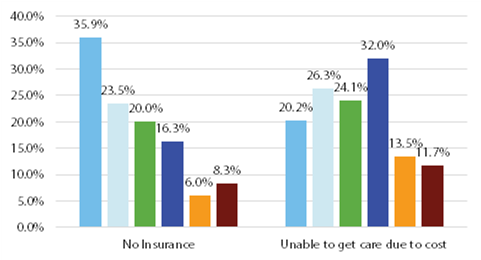
- Health care access and utilization—Health insurance rates vary widely by race/ethnicity as seen in Figure 1. More than 35% of Utah’s Hispanic/Latino population has no health insurance, compared with only 8.3% of the white population.[iii] Additionally, Figure 1 shows that cost frequently prohibits minority populations from receiving needed care.
- Work—People of color are more likely to be “essential workers” and work in settings such as health care, factories, grocery stores, and public transportation.[iv] This leaves them more vulnerable to COVID-19 exposure. Additionally, they are less likely to have paid sick leave and may be unable to afford taking time off.
- Education and Income—As a whole, minority populations are less likely to graduate both high school and college, leading to job options that are lower-paying, less stable, and less flexible. This can result in added stress, difficulty taking time off when sick, and challenges paying for needed health care.[v]
- Housing—Those from racial and ethnic minority groups are more likely to live in multi-generational or multifamily households.[vi] Additionally, rising unemployment rates due to the pandemic may exacerbate the issue by leading to increased risk of eviction, homelessness, or “doubling up” by sharing housing with family or friends. These crowded conditions increase risk of COVID-19 spread.
- Discrimination—Discrimination occurs across society and institutions, including in systems related to health and well-being (e.g. health care, housing, education, and criminal justice).[vii] Discriminatory experiences can lead to chronic stress and impact social and economic factors putting marginalized groups at increased risk for COVID-19 and other health conditions.
Figure 1: Access to Health Care by Race/Ethnicity, 2017–2019
Source: Utah Department of Health 2017–2019 Behavioral Risk Factor Surveillance System (BRFSS) Data
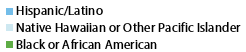
While COVID-19 is new to our society, racial health disparities are not. Social determinants of health disproportionately impact minority populations, leading to worse health outcomes in general. Table 1 provides a few examples. Prevalence of obesity/overweight, diabetes, and fair/poor general health are consistently higher among minority populations (with the exception of the Asian population). These chronic conditions put individuals at increased risk of COVID-19 complications and death.
Table 1: Prevalence of Selected Health Conditions by Race/Ethnicity, 2017–2019
*As compared to “good”, “very good”, or “excellent”
Source: Utah Department of Health 2017–2019 Behavioral Risk Factor Surveillance System (BRFSS) Data
While these disparities are long-standing, COVID-19 shines a spotlight on the issue. It underscores the need to improve access to health care and promote healthy behaviors. It also reminds us that health is multifaceted and impacted by more than a person’s interaction with the health care system. Education, employment, income, and housing are just a few examples of social and economic factors that impact health. Finding ways to address these social determinants of health will be a critical component in reducing racial and ethnic health disparities.
Andrea Thomas Brandley is a research associate at the Kem C. Gardner Policy Institute.
[i] Utah Department of Health as of October 16, 2020.
[ii] See https://www.cdc.gov/socialdeterminants/index.htm
[iii] Utah Department of Health 2017–2019 Behavioral Risk Factor Surveillance System (BRFSS) Data
[iv] U.S. Bureau of Labor Statistics. Labor force characteristics by race and ethnicity, 2018 [online]. 2019 [cited 2020 Jun 24]. Available from URL: https://www.bls.gov/opub/reports/race-and-ethnicity/2018/home.htmexternal
[v] Centers for Disease Control and Prevention (CDC). (2020, July 24). Health Equity Considerations & Racial & Ethnic Minority Groups. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html#fn17
[vi] ibid
[vii] See, for example, Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006; 35(4):888–901. DOI: https://doi.org/10.1093/ije/dyl056