Blog Post
Insight: COVID-19 Care Delays: Slowly Returning to Normal?
By: Laura Summers
Note: The opinions expressed are those of the author alone and do not reflect an institutional position of the Gardner Institute. We hope the opinions shared contribute to the marketplace of ideas and help people as they formulate their own INFORMED DECISIONS™.
One year ago, we were hit with the reality of living in a world with a spreading, unknown disease. We watched as other countries and states struggled with overwhelmed hospitals and health systems. Our local systems made decisions in response that would allow them to maintain capacity for critically ill patients, limit the spread of the virus, and protect resources such as personal protective equipment. This included temporarily restricting access to nonessential medical services and procedures.
Our local health systems made the best decisions they could with the limited information they had at the time. A year later, though, there are many lessons learned and increasing concerns over the pandemic’s longer-lasting direct and indirect effects. One of these concerns is the number of people who delayed―and continue to delay―seeking necessary or routine medical care. Delayed care not only triggers a pent-up demand for treatment but can also result in missed early diagnoses, leading to health conditions that are harder to manage, or even premature death for some patients.
To understand the magnitude of this concern, it is important to know the numbers. While researchers will be studying the effects of COVID-19 for generations to come, the U.S. Census Bureau began surveying the U.S. adult population to better understand the pandemic’s immediate social and economic impacts. The Household Pulse Survey is an experimental survey designed to “quickly and efficiently deploy” data collected on how the coronavirus pandemic has impacted people’s lives. The Household Pulse Survey gathers data on education, employment, housing, transportation, food security, and health issues, including information related to accessing medical care. More information on the survey can be found here.
When our local health systems began to resume non-urgent and elective procedures in late April 2020, 37% of Utah adults surveyed by Household Pulse indicated that they had delayed getting medical care in the last four weeks because of the COVID-19 pandemic (Figure 1). This is more than one in three Utah adults. The survey also asks the more direct question of whether someone needed medical care for something unrelated to COVID-19 but did not get it. In late April and early May 2020, 27% of Utah adults indicated they needed medical care in the last four weeks but did not get it because of COVID-19 (Figure 2). Utah’s rates are comparable with nationally reported rates.
Figure 1: Share of Adult Population that Delayed Getting Medical Care Because of COVID-19 Pandemic
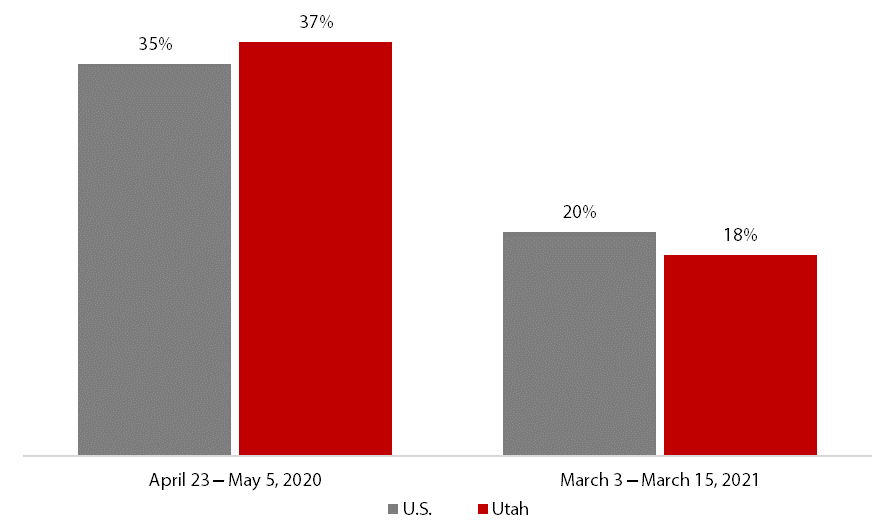
Note: Total population 18 years and older. These data are experimental. Users should take caution using estimates based on subpopulations of the data—sample sizes may be small, and the standard errors may be large.
Source: U.S. Census Bureau Household Pulse Survey, Week 1 and Week 26 (survey results are now collected and disseminated every two weeks).
Figure 2: Share of Adult Population that Needed Medical Care for Something Unrelated to COVID-19, but Did Not Get It
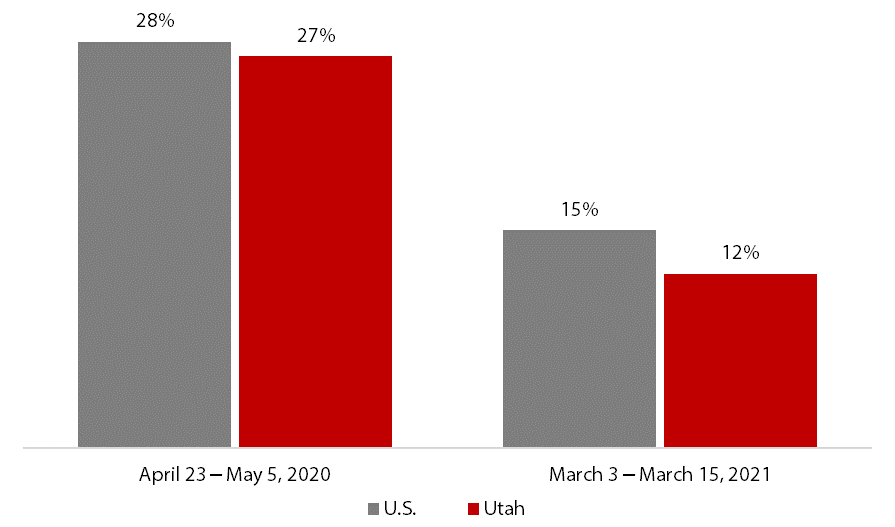
Note: Total population 18 years and older. These data are experimental. Users should take caution using estimates based on subpopulations of the data—sample sizes may be small, and the standard errors may be large.
Source: U.S. Census Bureau Household Pulse Survey, Week 1 and Week 26 (survey results are now collected and disseminated every two weeks).
Fortunately, the most recent data released from the Household Pulse Survey show that the percentage of adults delaying medical care has declined by more than half over the course of almost a year. This is a positive trajectory, but there is room for improvement. From March 3 to March 15, 2021, 18% and 12% of Utah adults, respectively, reported delaying or being unable to get medical care due to COVID-19.
Emerging research is already beginning to estimate the impact these delays in care could have on health outcomes. To mitigate these effects, our local health systems should continue to encourage people to seek timely and appropriate care, particularly now that policies and procedures are in place that allow people to safely access the medical system, even during a pandemic.
That said, more has to be done to address access than just messaging. COVID-19 is only one in a long list of reasons why people don’t or can’t access the health care system. Cost, lack of transportation, and lack of culturally and linguistically appropriate services are only a few of the most commonly mentioned barriers. COVID-19 was an acute disruption that led to a population-wide inability to access health care. However, solutions to the problems associated with delayed care should focus on the issues that existed before and will remain after the pandemic officially ends.
Laura Summers is the senior health care analyst at the Kem C. Gardner Policy Institute.

